Scabies Is Making a Comeback
Share- Nishadil
- January 17, 2024
- 0 Comments
- 9 minutes read
- 167 Views
Scabies Is Making a Comeback
Cases of scabies, a highly contagious parasitic skin disease, are on the rise across Europe. The UK in particular is struggling with a shortage of treatments.
In recent months, Naveed Ijaz, a general practitioner specializing in dermatology, has seen a growing number of patients presenting at his clinic in Manchester, UK, with intensely itchy rashes. Their cause is scabies, a highly contagious skin condition caused by the Sarcoptes scabiei mite, which can result in these itchy rashes spreading all across the body.
“I am extremely concerned, chiefly because of the shortage of treatments available,” says Ijaz. “Outbreaks tend to occur more so over the winter months, as people tend to spend more time together indoors. The shortage of available treatments compounds this.” While scabies is extremely common, affecting approximately 200 million people worldwide, cases across England are spiking far above typical levels.
Reports have detailed outbreaks in care homes and university accommodations, particularly in the north of the country. Emma O’Brien, a spokesperson from the UK’s Royal College of GPs, told WIRED that weekly incidences per 100,000 for the north of England continue to be well above the national and five year average.
Their most recent surveillance reports detailed 1,926 cases across the country between early December and January . The UK’s surge of cases is part of a wider, longer trend. Scabies cases have been rising consistently across Europe and around the globe for a decade. Unlike other infectious diseases, this isn’t thought to be a consequence of climate change, but a cocktail of factors—treatment shortages, treatment failure, and the persistent stigma surrounding the disease that prevents some from immediately seeking medical attention.
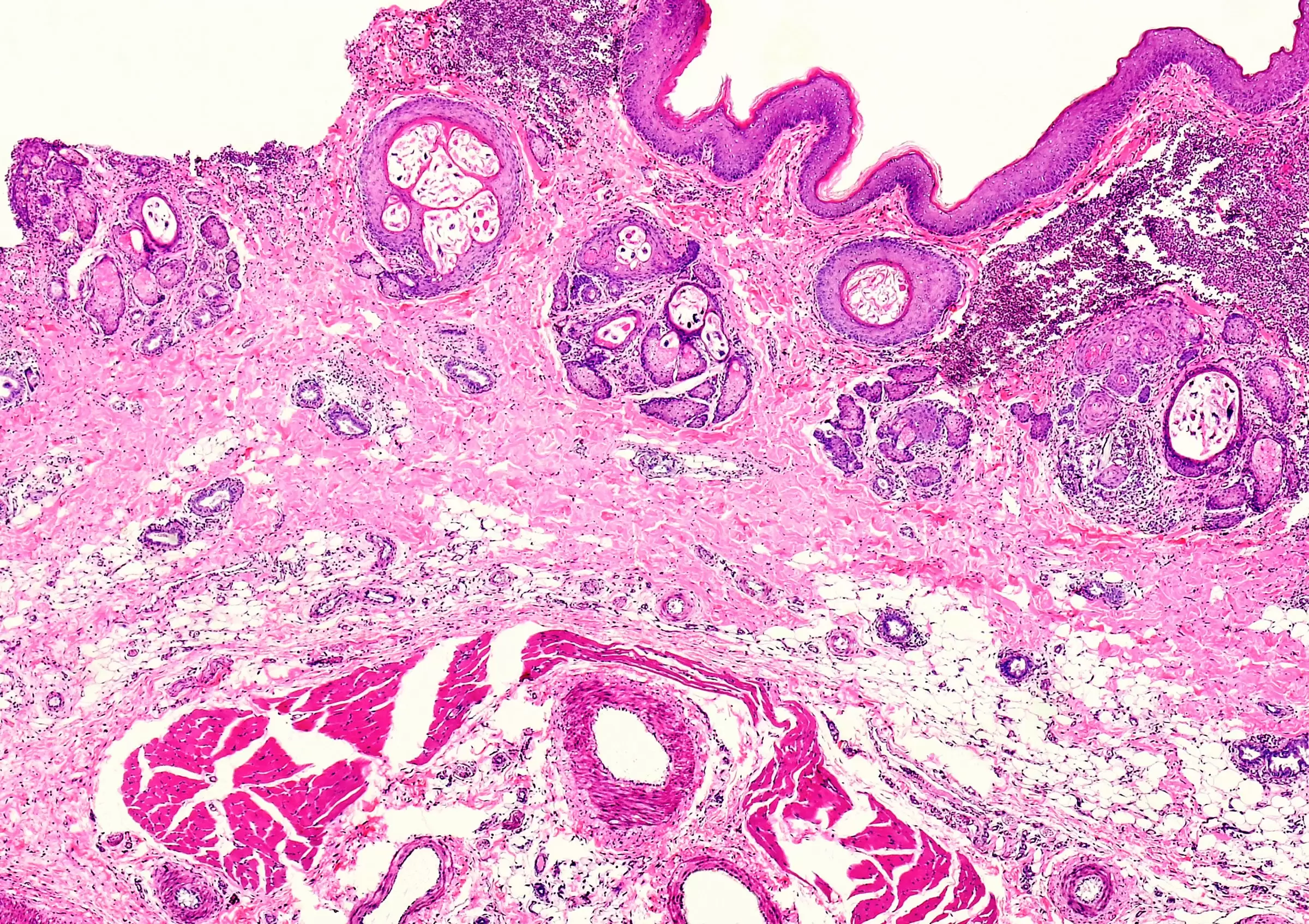
Until the condition is treated, scabies mites can reproduce, burrow, and lay eggs under the skin, causing sores and cycles of itching to continue. The mites can easily be transmitted to others, particularly through skin to skin contact—during sex, for example. Ijaz says he has seen several cases where individuals were infected by a sexual partner, while some of the data on the extent of the current UK outbreak has come from sexual health clinics.
“The mites can crawl off the human being and onto sofas or bedding, which is partly how outbreaks can be sustained,” explains Michael Head, a senior research fellow in global health at the University of Southampton in the UK. “It’s quite common in schools, prisons, and care homes, and we’ll sometimes see outbreaks in hospital wards or hostels.
The mite is relatively common, quite hardy, and alas for us, very good at doing its own job.” The two main treatments for scabies are permethrin and malathion, skin lotions that need to be rubbed across an infected person’s body to kill all the reservoirs of mites and eggs. Traditionally these treatments have been highly effective, but in recent years there have been growing reports of treatments failing.
A recent review of research on the topic, published by the British Journal of Dermatology , states that the treatment failure rate can be as high as 30 percent. The review notes that drug resistance among mites is an emerging concern, but also concedes that relatively little is known about this threat.
The high number of cases in the UK also reflects the difficulty of eradicating an outbreak, says Jo Middleton, a research fellow at Brighton and Sussex Medical School, who is involved in scabies research in the UK and around the globe. Bedding and furniture need to be completely decontaminated, while medicines like permethrin are not the easiest to use.
“Permethrin is a good medicine, but it’s very difficult to put on. You have to cover your whole body, leave it on for 12 hours without washing it off, and then you have to do it again seven days later,” he says. “The reality is that we see a lot of failure, where people put on this medication and end up continuing to have scabies and infecting other people, because the application is so difficult.” In Britain, there’s also another factor at play: a months long severe shortage of treatments.
Paula Geanau of the British Association of Dermatologists told WIRED in an email that this is due to both lingering pandemic related supply chain issues and import problems relating to Brexit. With the current high demand, any stock that reaches the UK is swiftly used up. “We’ve seen a shortage of pharmacy supply in some UK regions, particularly in the north,” says Middleton.
“It’s unclear what is causing which. Maybe there’s more cases, so therefore there’s a shortage in medicine, or it might be the other way around.” Researchers argue that given scabies’ relatively high incidence, there needs to be more rigorous surveillance of potential outbreaks, particularly in the wake of research showing that untreated scabies can lead to secondary skin infections from streptococcus and staphylococcal bacteria.
Vulnerable patients—in care homes, for example—are especially at risk, and these bacteria can even go on to cause organ damage. “There’s some links to the cardiac and renal systems,” says Head. “Not fully understood, but it does look like they are genuine, occasional secondary consequences of an initial scabies infection.” Scabies has long been neglected, perhaps due to the unhelpful stigma surrounding it as a “disease of the unwashed.” Rates have sometimes been reported as being higher in overcrowded conditions—in camps for refugees and asylum seekers, for example.
This idea may then be used to blame disadvantaged populations, without evidence, for spreading the disease. “I’ll strongly say there’s no evidence that any rise in scabies, if it is happening in Europe, is connected to refugees,” says Middleton. “There’s been stuff in the media in the past associating refugees with bringing scabies into a country, but scabies is here, and it’s always been here.
Where we see outbreaks is predominantly in care homes and among young people in universities. It’s what’s going on in those places that will explain any rise.” This isn’t the only piece of misinformation to swirl around the disease. In the global south, scabies is managed effectively through an oral medication, a powerful antiparasitic called ivermectin.
Studies have shown that two doses of ivermectin are effective at eliminating the disease in 98 percent of patients. Yet ivermectin is not routinely used to treat scabies in the UK, something that researchers attribute to the repeated false claims regarding its potential uses for treating Covid 19. At one point endorsed by former US president Donald Trump, ivermectin’s supposed usefulness against the SARS CoV 2 virus was never backed up with reliable evidence, and Middleton believes this is sadly now inhibiting its use in conditions where it is proven to work.
“Some people were claiming that it had efficacy against Covid,” he says. “To try and control that you had other people describing it as horse paste, because it is—like a lot of human medicines—also a veterinary drug. That then gave it a kind of bad reputation. But we are hoping it will be used more against scabies.” In the meantime, doctors such as Ijaz are hoping that the current outbreak in the UK can be managed through more effective public health campaigns.
“People can often be mismanaged,” he says. “For instance, itching post treatment can last anywhere up to six weeks post eradication, yet people mistake this for a recurrence of scabies. This leads to them sourcing more permethrin, leading to more shortages.”.
Disclaimer: This article was generated in part using artificial intelligence and may contain errors or omissions. The content is provided for informational purposes only and does not constitute professional advice. We makes no representations or warranties regarding its accuracy, completeness, or reliability. Readers are advised to verify the information independently before relying on







